You know that there's a lot of controversy about how to run a cardiac arrest - intubating or not, how often to ventilate, or doing a short trial of CPR before defibrillation. This is especially true regarding the "code drugs," like epinephrine.
 |
| Well, okay. Epi works. |
But at least when it comes to epinephrine and amiodarone, there are some studies out there, some base of evidence to start the discussion from. This is not true for D50.
If you look in the 2000 ACLS guidelines, you'll see the list of the "reversible causes" of cardiac arrest. It doesn't include hypoglycemia.
 |
| If you don't believe me, look at the fine print at the bottom. |
Now skip ahead 5 years, and we now see that hypoglycemia has been added (2005 ACLS):
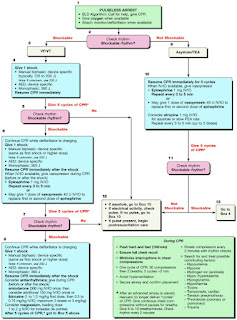 |
| Down in the green box, at the bottom. |
Read through the guidelines, though, and you'll see that not a word is uttered about why this was added.
Now, fast-forward to 2010, and they've taken it out! And, just like they added it without comment, it's gone without a trace.
 |
| Poof! |
Since the AHA elected not to review any relevant evidence about the topic, I decided to answer some questions about hypoglycemia, cardiac arrest, and the relative benefit of trying to squeeze that huge syringe of syrup into an IO.
1. Does hypoglycemia cause cardiac arrest?
You figure this would be easy enough to answer, but there is almost no direct data that says so. One case series in 1995 reviewed 3 arrests that the authors thought were associated with hypoglycemia. These patients all had significant other problems (active CAD, cerebral hemorrhage, and severe pancreatitis).
Another case series, looking at patients with severe heart failure, thought that one cardiac arrest was due to hypoglycemia (oddly enough, she didn't have diabetes). And in one last example, a patient in the ICU became asystolic at the same time her blood sugar was plummeting, although she also was developing a severe hyperkalemia at the same time.
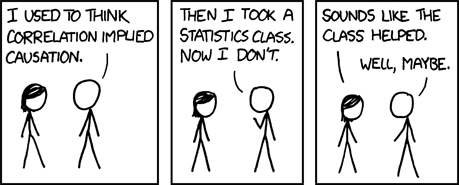
The problem with this handful of case reports is that, given the uncontrolled nature of the situations, it's hard to point out cause and effect. Just because one thing occurred at the same time as something else, or even right after, doesn't mean they're related.
Well, look at this from a different point of view. Is there a proposed "mechanism," some physiological reason that hypoglycemia could cause an arrest?
There is the phenomenon of the "dead in bed" syndrome, where a relatively healthy diabetic is found deceased in the morning. A number of researchers think they've found a link - the usual dip in blood sugar levels at night can cause a prolongation of the QT interval. And long QT intervals can sometimes cause problems! (See these examples at Dr. Smith's ECG Blog.)
 |
| A long QTc. (source) |
But, just because you can show a longer QT, doesn't mean you have a smoking gun! Others have pointed out that there are probably a number of other factors involved. For instance, it may not be the hypoglycemia that triggers the QT changes, but in fact may be the body's own epinephrine that kicks off the arrythmias!
 |
| Now epinephrine is bad for the heart?!? |
So, we just don't know!
2. Is the finger stick accurate in cardiac arrest?
Usually, the capillary blood glucose is pretty close to the venous level, close enough that we all trust it. However, in the critically ill patient, the capillary level becomes less accurate, as a number of studies have shown.
2. Is the finger stick accurate in cardiac arrest?
Usually, the capillary blood glucose is pretty close to the venous level, close enough that we all trust it. However, in the critically ill patient, the capillary level becomes less accurate, as a number of studies have shown.
Only one study looked at patients getting CPR, though. This was a pretty big study by cardiac arrest standards - they checked the venous and capillary glucose levels in 50 cardiac arrest patient. It wasn't encouraging. There were 4 patients with "true" hypoglycemia, found on the venous samples sent to the lab. The fingerstick missed 1 of those, and also managed to misdiagnose 5 patients as having hypoglycemia, when they really didn't. (The fingerstick was 75% sensitive, and 38% specific).
Not so accurate!
3. Okay, we might over-diagnose hypoglycemia. What's the harm?
Glad you asked.
It's the same reason we're trying to cool people down after we get a pulse back - neurologic outcomes. In some studies, they gave dextrose to some cats before they put 'em into cardiac arrest, while other cats they didn't. The cats who didn't get sugar beforehand had better brains afterwards.
You can't really do this same kind of study in humans (for example). One group in Helsinki, though, checked the blood sugar on VF cardiac arrests, and looked at how well they recovered. Patients who had increases in their glucose after resuscitation didn't survive to hospital discharge as often. This is just the latest evidence - see this review article (50% dextrose: antidote or toxin?) for plenty of other examples.
Not so accurate!
3. Okay, we might over-diagnose hypoglycemia. What's the harm?
Glad you asked.
It's the same reason we're trying to cool people down after we get a pulse back - neurologic outcomes. In some studies, they gave dextrose to some cats before they put 'em into cardiac arrest, while other cats they didn't. The cats who didn't get sugar beforehand had better brains afterwards.
You can't really do this same kind of study in humans (for example). One group in Helsinki, though, checked the blood sugar on VF cardiac arrests, and looked at how well they recovered. Patients who had increases in their glucose after resuscitation didn't survive to hospital discharge as often. This is just the latest evidence - see this review article (50% dextrose: antidote or toxin?) for plenty of other examples.
4. Any evidence giving sugar helps?
Well, yes and no. There is no evidence that pumping liquid rock candy into someone's tibia helps in cardiac arrest.
 |
| Medicine! |
Now, there are a lot of other sick people out there, people teetering on the edge, critically ill, septic, metabolically deranged - with a blood sugar headed south, and fast. You have to find those folks and treat them quick. Some of these are kids, with weird metabolic problems, or with sepsis. But the key is to get to them before they crash.
The authors of the only review I found on this topic concluded that (my emphasis):
It's in the protocols, you can certainly give dextrose if you think it's warrented. In he field, though, there's a lot to be done, and sometimes there's not enough hands to do the work. If there's enough crew around, maybe it's fine to dedicate one person to squeezing the D50 in. If space and time are limited, whoever, it's important to understand the effectiveness and and evidence for your therapies.
The authors of the only review I found on this topic concluded that (my emphasis):
"This is obviously a controversial issue and raises the point of whether we should still be teaching that hypoglycaemia is a reversible cause of cardiac arrest when there seems to be not enough evidence to support this.
Current evidence would suggest that patients may suffer cardio-respiratory arrest with hypoglycaemia, but not because of it."The Bottom Line
It's in the protocols, you can certainly give dextrose if you think it's warrented. In he field, though, there's a lot to be done, and sometimes there's not enough hands to do the work. If there's enough crew around, maybe it's fine to dedicate one person to squeezing the D50 in. If space and time are limited, whoever, it's important to understand the effectiveness and and evidence for your therapies.
Interesting topic presented wonderfully. We need more educators like this!
ReplyDeleteWell done. There isn't a lot of reason to give D50, well there isn't ANY reason to give D50 to a cardiac arrest patient. Now we're being told that we should check glucose levels post ROSC, but I'm skeptical. If too much oxygen post arrest is bad, and it is, why should we not think that too much D50 is bad post arrest?
ReplyDeleteYou betcha.
DeleteIf I write this up for a review article, I'll go over the evidence regarding glycemic management post-ROSC in more detail. Make it look all scientific and stuff. Suffice it to say, however, that your skepticism seems well-grounded.
I think this dextrose issue may be more relevant in the ED, where we seemingly have the resources to do "everything," whereas in the prehospital realm you have to really prioritize your actions.
It's funny you should mention that. During a recent ACLS refresher the instructor mentioned that post ROSC it would be helpful to do a BG reading. He wasn't adamant about it, but it was a "if you get to it" kind of thing.
DeleteHowever, during PALS a few days later, the instructor (a different one) was all over giving D25 to a pedi ROSC. She of course had no science to go with it, which is why I laughed at her.
I'll see her again Tuesday and laugh at her some more.
Ironically, she's originally from CT. Not that that has anything to do with it, but it appeals to my warped sense of humor.
And it's funny you bring up peds. I left it out of the post, but the pediatric evidence is no better, and even consensus is elusive.
DeleteCase in point: Compare the 2010 guidelines for peds resuscitation. In the AHA (PALS) guidelines, they describe hypoglycemia as one of the reversible causes (http://pediatrics.aappublications.org/content/126/5/e1361.full#sec-57).
In the international guidelines, however, there is no mention of hypoglycemia as a "treatable cause." (http://pediatrics.aappublications.org/content/126/5/e1261.full#content-block)
The funny thing is the lead author (Kleinman) is the same for both guidelines. Huh.
As for CT, we in the Nutmeg state care deeply about dextrose. Very deeply.
Brooks I know this is a old post but is is really informative. I cracked the books again to prep for a PALS course today and was reviewing H's and T's for peds and low and behold, like your last response Hypoglycemia is in there. Oddly I was debriefing cardiac arrests for the department and had just reinforced that hypoglycemia is not a "H" in ACLS 2010 guidlines. I have been fighting this hypoglycemia zombie (2005 guidelines) for months so was shocked to see it as a PALS H & T. I pulled the 2010 guidlines for CPR and ECC and read the passage related to it.
ReplyDelete"Because infants have a relatively high glucose requirement and low glycogen stores, they may develop hypoglycemia when energy requirements rise."
Ok I buy that but the leap of logic to next sentence is HUGE;
"Check blood glucose concentration during the resuscitation and treat hypoglycemia promptly" (Class I, LOE C)
They site this study for the reason- Derangements in blood glucose following initial resuscitation from in-hospital cardiac arrest: A report from the national registry of cardiopulmonary resuscitation☆
Interesting that this is retrospective study of adults.
Their conclusions:
Hyperglycemia is common in diabetics and non-diabetics following IHCA. Survival odds in diabetics are relatively insensitive to blood glucose with decreased survival only associated with severe (>240mg/dL, >13.3mmol/dL) hyperglycemia. In non-diabetics, survival odds were sensitive to hypoglycemia (<70mg/dL, <3.9mmol/L).
I don't see the correlation to warrant treating intra-arrest in infants when we cannot rely on our devices to even measure properly in the field. At best this seems to be best left to the hospital to correct post arrest. This seems to stretch level of evidence C to its breaking point.
Have you heard of any recent studies that may warrant this treatment? Perhaps a study in children.
As I recall, there were a few pediatric case series that featured critically-ill children who were noted to be hypoglycemic prior to arrest. (Not sure of the exact references, have to look through my PDF pile!) Whether this reflects a predisposition of the pediatric heart to arrest when hypoglycemic, or whether critically-ill kids are simply more likely to be hypoglycemic, it's hard to say.
DeleteBasically, I think we're all looking at the same pile of studies, but certain groups (adult, pediatric, and international) view them in slightly different ways.
Interested to see if it shows back up with the next acls update comming out soon
ReplyDeleteThe coincidences that lead me to this blog are innumerable, mainly that I came across it while researching this topic for a Bridgeport Hospital publication. As always, your insights are spot on!! You never cease to impress me, Dr. Walsh!!
ReplyDelete