 |
| Not filed under "valuable new studies": Leg-compression CPR |
I just wrote about EMS and cervical spine trauma. However, a new study deserves attention for a few important reasons.
First, it describes a simple method of assessment. Second, it "fits" with common sense.
Lastly, one of the co-authors is a Bridgeport Hospital ER doc!
 |
| Dr Althoff (Note: does not usually dress like the Unabomber at work) |
There has been a lot of discussion about how to "clear" the potential cervical-spine injury in the field. Some people like the simplicity of the NEXUS criteria, while other think that the Canadian C-Spine Rule (CCR) is more sensitive, and thus safer.
The use of these rules, though, can get complicated and confusing, with people arguing over how to define "intoxication" (when using NEXUS), or what is a "dangerous mechanism" (when using the CCR). Also, if the patient describes paresthesias, or insists that their neck is tender, despite an exceedingly minor mechanism, you may be obligated to immobilize.
Researchers at the University of Virginia decided to try a different approach - instead of examining the patient who has been in a MVC, how about just examining the car?
 |
| The stupidest clip-art I could find with Google Image |
The "Glass Intact Assure Safe Cervical Spine Protocol" study
The researchers used a national database of MVCs that had been reported to police, where at least one of the vehicles had been towed from the scene. The vehicle had all received a complete, systematic survey for damage afterwards by the NASS investigators, using both crash-scene photos and reports collected by police, as well as direct inspection of the vehicles. In addition, federal researchers combed over medical records to determine whatever injuries the occupants had suffered.
The Virginia researchers then looked at a subset of the patients in the national database:
- Ages 16-60,
- Had been wearing setbelt,
- Airbags did not deploy,
- All the car windows were intact
Well, it wasn't many. Out of 7639 drivers or passengers who met the "GLASS" criteria, only 6 had an unstable cervical spine fracture - that's 0.008%. Really, really infrequent.
Is this protocol ready to use?
Not quite yet, but it's promising.
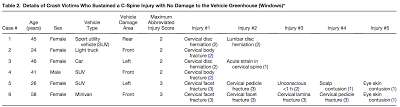
Keep in mind that this used a retrospective design, and a prospective design might look better or worse. And although there were very few injuries, they were serious. Here's a breakdown of those few, unlucky, patients with a spine injury after their minor (to us) MVC:
It's tough to draw any conclusions about these "potentially-missed" neck injuries You might be tempted to pay special attention to middle-aged females, but the (very, very) small sample really doesn't let us conclude much.
Nonetheless, the negative predictive value (or NPV) is astoundingly reassuring, with a confidence interval 99.86% to 99.98%. That's about identical to the NEXUS rule-out criteria, and much better than many other rules in emergency medicine (e.g. the PERC rule).
Perhaps the biggest strength of the study is the number of MVCs studied. There is no way that the Virginia researchers could have investigated 14,000 MVCs on their own. Although you always have to worry about the quality of any one individual data-point in such studies, the mass of data enables us to identify important effects that would not be identified in smaller (although supposedly more high-quality) studies.
The Bottom Line
The next time you pull up to an MVC, and you see all the car windows intact, you can check the results for yourself.
But you still better go ahead and talk to the patient and do a physical exam!
Questions for one of the authors?
I've talked with Dr Althoff about this study on a number of occasions, EMS spinal care in general, and also future directions for research in this area. If you have questions about this study, or a related topic, send in a comment!
I am of several minds about this. Although I love to see more research on spinal immobilization -- especially ways to avoid doing it -- and it's interesting that they tried to use objective criteria, I can't help but feel like further glorifying mechanism is not a positive step, and the criteria seem a little arbitrary.
ReplyDeleteWhat I think this reveals more than anything is that almost nobody with a stupid (technical term) MVA mechanism has a significant spinal fracture, so just about any criteria to rule them out will have pretty good specificity. I wonder what the numbers would've been if they'd used, say, the presence of over $1.00 in change in the seats.
My other complaint is my standard one, which is that the entire game is predicated upon assumptions which may not have a basis in reality. If those are "significant" spinal injuries (in the chart), we're meant to view them as the misses, but by what lights are we calling them "unstable"? The fact that they would eventually require operative fixation? Because what we instinctively read is that these people were at risk of deteriorating prior to hospital arrival without spinal immobilization, and that's probably a huge leap.
I wouldn't take lack of airbag deployment as arbitrary, since there is a quantifiable force associated with activation - or at least there is supposed to be! As for the windows, glass tends to break if sufficient force is transmitted to it.
DeleteSpare change, on the other hand, is only associated with mild, and disproportionate, feelings of victory.
Cervical trauma requires, well, trauma. If there are not signs of significant trauma to the vehicle, do we still need to immobilize?
(Well evidently, some British EMS officers believe so... http://www.bbc.co.uk/news/uk-england-sussex-20944339)
Well, no doubt. But we can probably all agree that vehicle damage is, at best, a somewhat indirect and poorly-predictive indicator of patient injury. My point is, the prevalence of this disease is going to be so low that it's probably not hard to find criteria which yield a pretty good predictive value, and in the end I suspect that clinical criteria are a better choice than mechanism-based criteria -- even if they tend to be more subjective and hence with less interrater agreement.
DeleteI mean, what's our goal here? To come up with something that's so easy to use, a caveman could do it? Are the other criteria really so subjective that it's a problem?
Gah I'm a week behind on my reading - it might as well be a year in FOAMed time.
ReplyDeleteI tore into, in my opinion, an overly-glowing review of the study on JEMS (http://www.jems.com/article/patient-care/analysis-supports-limiting-spinal-immobi), but I've really been trying to like it over the past couple weeks. There's still two things I can't get over:
1) Like Brandon said, the focus on the mechanism involved in the collision at the expense of patient assessment. I don't know if I would ever feel comfortable clearing a NEXUS-positive patient in the field, even if they were GLASS negative. On the other hand, if they are GLASS negative and NEXUS negative, you really haven't gained anything over just using NEXUS. The only real utility I see would be in the altered patient for whom NEXUS does not apply, but that's going to require a lot more evidence of safety, which leads nicely in #2...
2) One of the things that makes NEXUS so special is the pains that researchers went to achieve good follow-up when it was being validated. Being retrospective registry data, that kind of follow-up is just not assured and worries me when we're talking about rare-but-devastating consequences. I've looked through the registry they cited, and although a lot of the collision info is detailed and well documented, the medical follow-up is a bit less trustworthy. There could have been six bad outcomes or there could have been sixty - it's a classic "unknown-unknown" per Rumsfeld.
I give the authors kudos for diving into the data to find a novel and objective demonstration of a low-risk mechanism, but until there's prospective validation done I think this paper has gotten all the attention it needs. Hopefully it won't affect my practice, but I have a feeling I'm going to be paying extra attention to vehicle windows when I'm in the field - pretty well matching your summary.
Of course my whole discussion above is looming under shadow of the bigger question, which is "Do any non-obtunded, neurologically intact patients even need C-spine immobilization?" Obvs we don't know the answer, but I meant to throw that in...
DeleteAll auto glass is not created equal. The windshield in modern vehicles will break far more easily than the side or rear windows. You can whack you head on the side glass pretty hard and the glass will not break.
ReplyDeleteIf the glass is broken for reasons other than a patient's head contacting it, it does signify a pretty good amount of force was applied. Think roll over.
Still, if mechanism is a poor prognosticator of injury, it's an equal poor prognosticator of lack of same.
I think that examining the patient, or rather teaching EMTs and paramedics how to properly examine a patient for injury is the way to go.