*** ACUTE MI ***
you can take that to the bank.
This hasn't fit with my experience, and so I was very interested in Peter Canning's latest post, since it validated my suspicions. He found that the ECGs his system are acquiring show surprisingly poor sensitivity and specificity for STEMI, if you simply rely on the computer to diagnose.
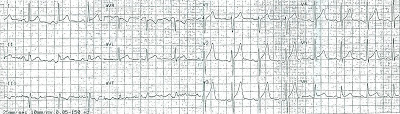
As an illustration of this point, I submit ECGs from 2 patients.
(For more pairs of ECGs that show the problem with relying on the computer diagnosis of STEMI, click on the label "Paramedics need to read ECGs..." on the right.)
Case 1
Let's say that this was a middle-aged female, who started having substernal chest pain about 15 minutes ago. The EMS 12-lead shows:
Aside from diagnosing the patient as "borderline," anything else look suspicious?
Case 2
Again, a middle-aged female, this time with pleuritic chest pain and wheezing. An ECG obtained 5 minutes after arrival in the ED shows:
What's an appropriate next step? Call in the (cardiology) cavalry, or do a little sleuthing?
 |
| Call for a bat-stent? (source) |
If you look closely at few of the leads, especially V3, you can see small spikes preceding the QRS. Since the computer hadn't seemed to notice, I adjusted the settings to recognize pacemakers. A second ECG then showed pretty much the same complexes, but a very different interpretation.
 |
| Fixed! |
How about case #1?
Evidently the patient was first transported to a non-PCI capable hospital. About 2 hours later she was on her way to a different hospital for an urgent cardiac catheterization. This gave EMS a unique opportunity to capture the evolution of the ECG over a time frame that we don't often find in urban/suburban EMS.
Frankly, I'm inclined to agree with the computer this time! But what did the computer "miss" on the first ECG?
Hyperacute T waves
As Peter found after analysis of his system's STEMIs, computers aren't good at recognizing the earliest sign of an MI on an ECG, the hyperacute T-wave. These are transient features, before the ST segment has had a chance to elevate, and EMS is in a unique position to find these on their initial ECG.
Stephen Smith has some great examples, some of which look very similar to case #2 here. For instance, this ECG was acquired by EMS, and was instrumental in suggesting ACS to the emergency physician:
 |
| Dr Smith's ECG Blog - 6/2011 |
 |
| Dr Smith's ECG Blog - 2/2009 |
The Bottom Line
For more teaching on hyperacute T-waves, follow the links above to the blogs written by Peter Canning or Dr Smith, or check out this review.
And remember - sometimes you have to treat the monitor, not just the patient. Just make sure you're not treating a mistaken computer!



Are there set variables that define "hyperacute T waves" IE; t wave amplitude > 1/2 height of QRS in lead "x", or is this entirely based on clinician gestalt?
ReplyDeleteThe definition of hyperacute T waves hasn't been well-worked out. Many references use an absolute cut-off; Marriott's uses > 1.4 mV in V2 or V3.
DeleteThis seems incomplete, since so many other ECG definitions use relative definitions: the degree of expected STE in LVH, the "Smith criteria" for STEMI in LBBB, as well as ST/T amplitude in pericarditis.
One study suggests that relative cut-offs might be useful in this area as well, and I talk about a single retrospective study, so-far unvalidated, that derived some such criteria. See my FB post that goes over this study:
https://www.facebook.com/photo.php?fbid=356252804476950&set=a.281990401903191.48279.145223525579880&type=1
Of note, though, ECG #1 in this post only meets 2 out of the 4 criteria that the study derived. With that in mind, I think clinician gestalt still has a huge role. (Or 20/20 hindsight!)
I was not sure if love spell could help but here is my story:
ReplyDeleteI have been in a relationship with my then ex (we broke up for 3 months) since 2017. It was a happy and very active relationship with lots of fun and travelling. We love each other endlessly and we shared a lot. His family was my family and my family his.
Few months back he started being controlling and possessive:
I told him that I don’t feel comfortable with his new behavior, he apologized and promised to work on himself. But he failed on his promises, this time it escalated to him being manipulative. He accuses me of cheating on him at work. Eventually, I’ll be the one apologizing for something I didn’t do. I broke up when I couldn’t take it any longer.
I got a stranger email address from a website that changed my story:
I asked the stranger for help to fix my relationship, I told him that my problem was that I am still in love with this guy and I know he loves me too but he has a huge ego, his ego is enormous. I know I am the one who did the breaking up but my heart was hoping for him to say to me ‘I’m sorry baby, I apologize for how I have made you feel these past years, I will seek help and fix myself so that we can fix us’
The stranger is Dr. Mako, his email; Makospelltemple@yahoo.com
Dr. Mako showered his healing powers to us through his powerful love spell. Our relationship was fixed as he provided the much-needed help to us. Our destiny was changed for good.You can also contact him on his WhatsApp Number:+2347054263874
I really want to thank Dr Emu for saving my marriage. My wife really treated me badly and left home for almost 3 month this got me sick and confused. Then I told my friend about how my wife has changed towards me. Then she told me to contact Dr Emu that he will help me bring back my wife and change her back to a good woman. I never believed in all this but I gave it a try. Dr Emu casted a spell of return of love on her, and my wife came back home for forgiveness and today we are happy again. If you are going through any relationship stress or you want back your Ex or Divorce husband you can contact his whatsapp +2347012841542 or email emutemple@gmail.com website: Https://emutemple.wordpress.com/ Https://web.facebook.com/Emu-Temple-104891335203341
ReplyDelete