Frankly, a kid who faints is not the most interesting patient. Young ladies have a habit of swooning, especially if Justin Beiber is involved. As for young guys, they are hardly immune:
So it it usually isn't too exciting to be called for a 14 year old girl who had fainted. Usually.
The Patient
During the evening she had been feeling an upset stomach, describing some epigastric discomfort, as well as nausea. Her parents remember that she looked a little pale before the episode ocurred. She was walking into the kitchen when she began to feel faint, and was seen to fall onto the floor. Her parents, frightened, called 911 immediately.
The ALS crew found her sitting up in a chair, a tissue held up to a small cut on her forehead, but otherwise looking well. Vital signs were normal, and the parents were starting to feel like they had been overreacting in calling 911. While sitting in the chair, however, she suddenly stiffened up her whole body, and then went limp. After being put on the floor, she regained consciousness. Although she came around quickly this time as well, everybody decided that calling 911 had been just fine, and she was moved to the ambulance for transport to the ED.
During transport, the medic noticed that her heart rate was slowing down episodically, dipping into the 40's. She still looked pale, and vomited a few times, but her mental status was fine, and she never became hypotensive. A rhythm strip was obtained:
An ECG was also acquired:
The transient episodes of bradycardia did not require pacing or medication. She was brought into room 4 (our trauma/acute resus room), looking a bit intimidated by the number of nurses and doctors around her. She still looked pale, but her speech and mentation were normal. Naturally, we acquired an ECG immediately (about 30 minutes after the EMS ECG):
Vital signs were P-100, R-20, BP-127/59, SaO2-100% RA. Her lab work was uninteresting, and a CT of her head show no fractures or bleeding. The cut on her face needed only some Dermabond.
ECG analysis
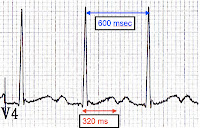
The ECG and rhythm strip obtained by EMS were acquired only a minute apart. The rhythm is interesting, showing a sinus rate of around 120, but with a 2:1 AV block, so that the ventricular rate averages 60. On the rhythm strip we see two episodes of more advanced AV block, with 3:1 conduction, while on the 12-lead we see an apparent Wenkebach pattern in complexes 5-9, with a progressively lengthening PR interval. The QTc, fortunately, appears normal, and there are no signs of pre-excitation, Brugada, or arrhythmogenic right ventricular dysplasia.
The ED ECG shows, first of all, how frakkin' important it is for EMS to grab ECGs in the field, since a number of features had changed on the ED tracing. In the ED there is only a mild 1st-degree AV block (214 ms), and no sign of Wenkebach phenomena. The computer read the QTc as 441 ms, "borderline prolonged," and it does appear to violate the "half the RR interval" rule for a normal QT.
 |
| https://www.kg-ekgpress.com/ |
Hospital course
Our patient was continued on cardiac monitoring during her hospital admission, but 24 hours of telemetry revealed only a single further dropped beat, as well as a resolution of her PRI prolongation. Tests for Lyme, as well as rarer infectious causes of AV block or myocarditis, were negative. She was due to start a Holter study upon discharge, and follow up with a pediatric cardiologist.
 |
| Turns out HIPPA does not apply to dogs, so I can show you a canine Holter monitor. |
1. Was this a seizure or what?
Although the second episode of syncope this young lady had began with an apparent seizure, it was unlikely to represent a primary neurologic process. First of all, the seizure was described as a brief whole body stiffening, follow by loss of tone. While some forms of epilepsy may manifest in this manner, it would be unusual. Also, there was no post-ictal confusion described by the paramedic or parents, making a "true" seizure unlikely. Other historical and exam findings also weigh against a seizure. A good illustration of other factors to consider are found in this article "Seizure versus syncope (PDF download), which features a handy guide:
So this was likely a "convulsive" sub-type of syncope (brief myoclonus due to low blood flow to the brain), following the flowchart above.
2. Ok, it's syncope - what kind was it?
Reading the textbooks, there are dozens of terms to describe the various supposed kinds of seizures; micturation, situational, vasovagal, neurocardiogenic, autonomic, reflex... you get the idea. Really, there are only two types of syncope out there, from an EM/EMS point of view; cardiac or non-cardiac. Let's start with the second.
"Non-cardiac" does, of course involve the heart, but it's role comes in at the end of a sequence of events which are, as usual in medicine, not well worked out. The standard explanation sounds so weird, it may even be true.
For whatever reason, the body can pool blood excessively in the lower extremities. To compensate, both vascular tone and cardiac output increase substantially. Unfortunately, various pressure receptors in the heart now think the body is hypertensive, and act as if the patient has high intercerebral pressure; the heart rate drops, and cardiac output falls.
The fall in heart rate and blood pressure appear to be mediated by the vagal nerve, at least in part, so people call this vasovaagal syncope. On the other hand, since the sympathetic pathway is also affected, others call this autonomic syncope. Of course, as the picture above shows, the brain has a role in this, so it also called neurally-mediated syncope. If bardycardia, or even asystole (transient), are the main manifestations, it may be termed cardioinhibitory, but if hypotension is prominent, it can be instead called vasodepressor syncope.
Whatever. The important point is to distinguish these benign types from cardiac causes. This kind of "syncope" is caused by a primary problem within the heart, and may not produce all the autonomic symptoms (sweating, warmth, nausea) that normal syncope does. It comes on fast, and can occur even if the patient is seated or supine. This table from a Nadas' Pediatric Cardiology reviews the differences with normal, or "neurally-mediated" syncope:
Remember how normal syncope has a bunch of vague terms to describe the same thing? In contrast, there are 3 clear types of cardiac syncope, with clearly defined etiologies.
First, there are structural causes (hypertrophic cardiomyopathy, tetrology of Fallot, pericardial tamponade, amongst others).
Next, tachyarrythmias can induce syncope. Examples include long QT, Wolf-Parkinson-White, and Brugada.
 |
| I calculated 411 msec. Normal |
Last, but certainly not least, we have to worry about bradyarrythmias - sick sinus syndrome, overdose of beta-blockers, and, of course, advanced AV blocks!
3. Finally! So, did the AV block cause the syncope?
Well, that is the main question!
Let's consider a few factors in answering. First, our patient is young and otherwise healthy - she is old enough to be fairly sure she doesn't have an undiagnosed heart defect, but young enough that she hasn't had a few infarcts take out her conduction system. Right off the bat, it seems unlikely she could have some intrinsic heart disease causing her syncope.
Next, her presentation fits with a vasovagal/neurally-mediated/autonomic syncope. Look back up at the table above - she had some lightheadedness before she syncoped, she felt cold, had no history of syncope during exercise, and it occurred while she was standing (although the second event happened while seated upright). She looked pale afterwards, and felt nauseous for a time afterwards.
Lastly, we know that her ED ECG was almost completely normal, and an ECG the next day showed resolution of the PR interval prolongation. For all these reasons, it seems unlikely that she had some cardiac disease - structural or dysrythmic - that produced the AV block. Most of those problems don't disappear overnight.
4. How often do you see AV blocks in syncope?
Not too often, but it happens.
In a recent study (Electrocardiographic characteristics of atrioventricular block induced by tilt testing.), researchers noted looked at patients who had been put on a tilt-table to investigate the cause of their fainting. The idea is that through putting the patient through a fancier version of doing orthostatic vital signs, we can provoke and replicate a syncopal episode. Now, it's not a perfect test, with plenty of false-negatives and false-positive, but it is lot less hassle than the alternatives.
 |
| Looks more like a catapult. Just sayin'. |
The AV blocks didn't last long, less than a minute, on average. The majority of these patients had some form of second- or even third-degree block, as well as having significant periods of ventricular aystole!
A few key results from this study suggest that our patient had a faint causing her AV block, rather than the other way around.
First, they found that patients in their study had PP intervals that varied significantly. This is subtle, but can be appreciated on the EMS rhythms strip.
If you use the interval between the 2 non-conducted P waves as the standard (5th arrow), it's clear there is some PP variability on this strip.
Next, they found that these AV block developed gradually, usually after PR interval prolongation. We can see this variable on the EMS 12-lead:
5. What did the cardiologists diagnose her with?
They felt this was all likely due to "hypervagal tone," perhaps provoked by some mild hypovolemia. The results of the Holter study are pending.
Wrapping it up
EMS is in a privileged position, able to evaluate these patients within minutes after their episodes. You may be able to evaluate cardiac events that we might not ever see otherwise. This was a healthy young lady who had some pretty rare features of a common condition. It would have been easy to "BLS it in," and not get an ECG, or even a rhythm strip. Without a thoughtful medic in the back of the rig it may have missed entirely.









I started on COPD Herbal treatment from Ultimate Health Home, the treatment worked incredibly for my lungs condition. I used the herbal treatment for almost 4 months, it reversed my COPD. My severe shortness of breath, dry cough, chest tightness gradually disappeared. Reach Ultimate Health Home via their website www.ultimatelifeclinic.com I can breath much better and It feels comfortable!
ReplyDelete
ReplyDeleteI was diagnosed with COPD four years ago and struggled with worsening symptoms despite using inhalers and medications. Last year, I tried a herbal treatment from NaturePath Herbal Clinic, and to my surprise, it made a huge difference. My breathing improved, the coughing eased, and my energy came back. I feel better than I have in years. If you're dealing with COPD, I highly recommend checking them out: www.naturepathherbalclinic.com.